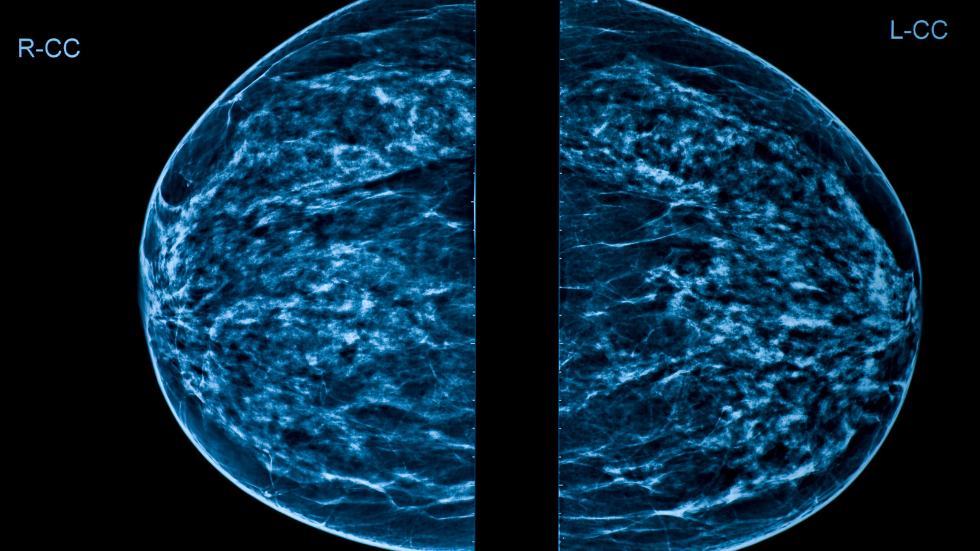
Mammography can pick up cancers 3 to 5 years before people can feel it with their hands. It can detect the earliest types of breast cancer, stage zero, which are usually micro-calcifications. Currently, 3D mammograms are the newest and latest technology that allows us to view the breast layer by layer, instead of just looking at the top to bottom, side-to-side view of the breast. This tool is especially helpful for people who have dense breasts.
Black women have up to 21%- 31% greater breast density compared to their white counterparts and also have a higher mortality compared to almost every other race and ethnicity. Ultrasound can be helpful as well for women with dense breasts to help differentiate between normal spongy tissue and an actual mask. Women who have heterogeneous, 50% or more dense breast tissue, might benefit from a whole breast ultrasound.
Having dense breasts shouldn’t be alarming, though it should spark questions with doctors to determine what your breast density level is, whether you are at elevated risk, how to personalize screening based on that risk level, and what type or additional imaging you should perform.
Generally, women at average risk should start getting mammograms at 40 years old every year until their life expectancy is less than ten years. According to the National Comprehensive Cancer Network (NCCN) guidelines, risk assessments and conversations about screenings should start as early as 30 years old – open the line of communication with your families and your physicians to determine what your risk level is, and what works best for you.
If women are at average risk and have no family history of breast cancer or history of breast biopsy showing atypical or abnormal cells, I recommend that they start at age 40 and perform it every year. If they wish to start earlier, especially if they’re women of color or if their breasts are at 50-75% density or higher, they can talk to that doctor and might need to get an ultrasound. Women who are at higher risk should start talking to their doctors in their thirties and familiarizing themselves with self-exams.
Women should assess their personal risk factors with their doctors and decide on the right imaging and the right screening for them. If their lifetime risk for breast cancer is more than 20%, they meet the criteria for a mammogram and MRI twice a year. Family history is one of the big determinants to determine whether a person is at high risk. If a person has a family history of breast cancer, their screening should start ten years younger than the youngest person in the family.
Pain is uncomfortable, and anticipation of this pain is one of the biggest reasons behind women not getting a mammogram. The mammogram process involves compression, which might cause a little discomfort. As women go through mammograms, they are also worried about the amount of radiation, but mammograms have low radiation exposure, and their benefits outweigh the risks.
Sometimes, women fear mammograms because they are concerned about finding “something” from the results, and then being followed up with either an additional biopsy or another doctor appointment. Our goal as healthcare providers is to catch cancer quickly. Technologies used in this detection are better than it’s ever been so if we find “something,” we want to rule it out and get involved early to keep women healthy.
Women should practice breast self-awareness, meaning that they should conduct a self-breast exam every day, before, during, and after a menstrual cycle or even if they’re perimenopausal or postmenopausal, because we know that hormones influence the changes in our breasts.
There are three parts to the self-exam – looking in the mirror, examining yourself while standing up, and examining yourself while lying flat. Oftentimes, we taught women to feel for lumps but not for normality. However, lumpiness can be normal and if not sure, they can ask their doctor to understand the normal architecture of their breasts.
Increasingly, young women are the fastest-growing population who get breast cancer. Self-care is not selfish, and it is a part of self-care to #CheckYourBreast, #CheckYourChest, and consider getting breast screened every year, depending on your individual risk factors.